Waterlogged
1
View details
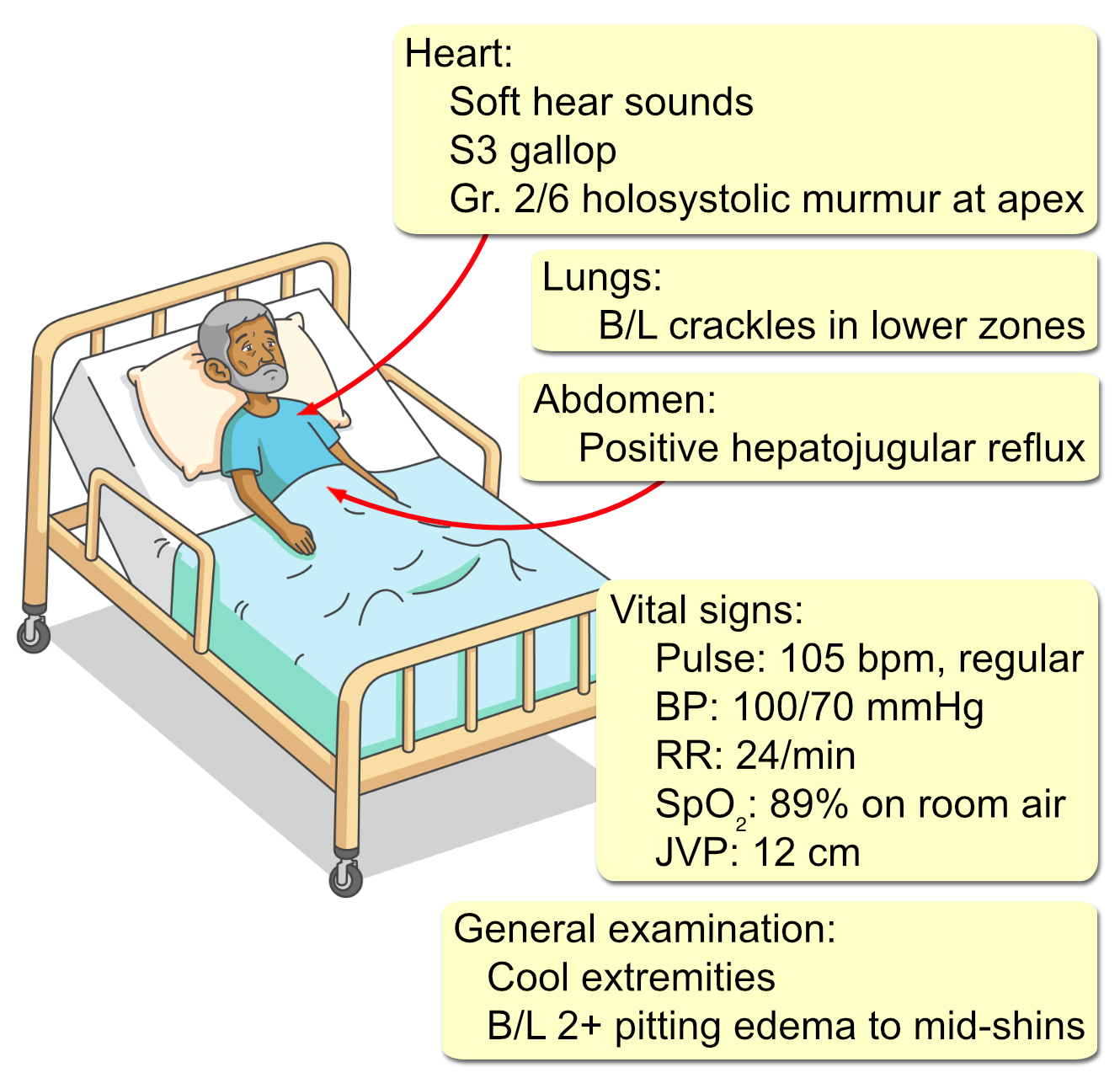
A 68-year-old man with a history of heart failure presents to the emergency department with 5 days of worsening shortness of breath. He now feels breathless even at rest and reports needing three pillows to sleep, up from his usual one. He has also been waking up at night gasping for air. His ankles are markedly more swollen than usual. He admits he has not been taking his prescribed diuretic for the past week and has been eating high-sodium takeout meals frequently. He denies chest pain, fever, or cough. His medical history is significant for ischemic cardiomyopathy with a left ventricular ejection fraction of 35%, diagnosed after a myocardial infarction 6 years ago. He also has hypertension and stage III chronic kidney disease. His home medications include lisinopril, metoprolol succinate, spironolactone, and furosemide. Initial laboratory studies are as follows:
WBC: 9,800/mm³ (4,500-11,000)
Hemoglobin: 12.1 g/dL (13.5-17.5)
Platelets: 210,000/mm³ (150,000-450,000)
Na+: 132 mEq/L (136-146)
K+: 4.1 mEq/L (3.5-5.0)
Cl⁻: 94 mEq/L (98-107)
HCO₃⁻: 26 mEq/L (22-29)
BUN: 45 mg/dL (7-18)
Creatinine: 1.8 mg/dL (0.6-1.2) [Baseline 1.4 mg/dL]
Glucose: 120 mg/dL
NT-proBNP: 6,500 pg/mL (<300)
Troponin I: 0.08 ng/mL (<0.04)